Cataract Eye Surgery

What Do You Understand By Cataract?
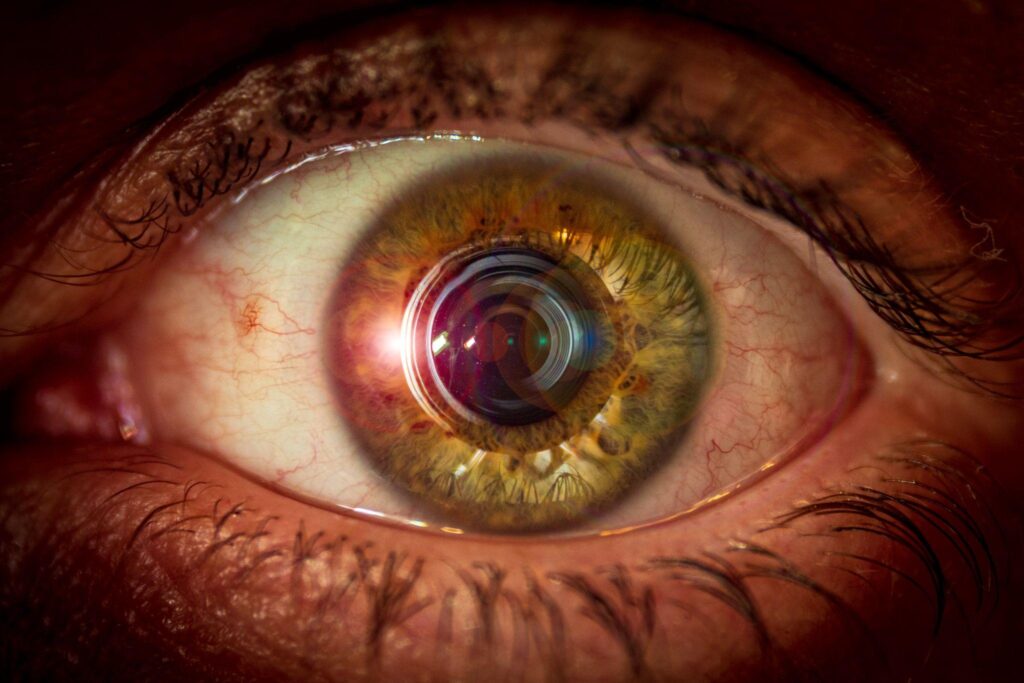
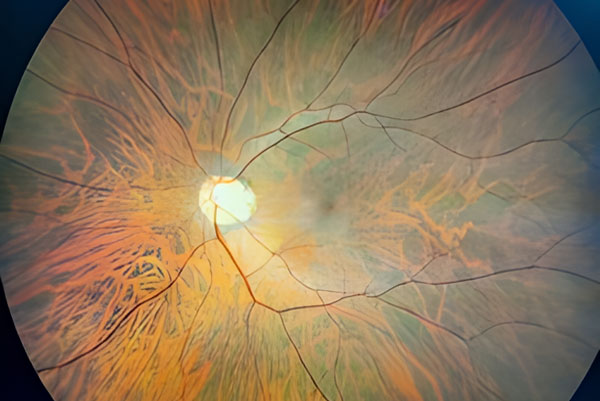
A cataract is a cloudiness or opacity of the eye’s natural clear lens. It obstructs the passage of light to the eye’s retina and impairs vision. When the lens develops cloudiness to the point that it impairs vision, it is called Cataract. It is like looking through a frosted glass.
What causes cataract?
Cataracts occur when there is a buildup of protein in the lens that makes it cloudy. This prevents light from passing clearly through the lens, causing some loss of vision. The common causes of cataract are:
- Age related (most commonly)
- Steroid use
- Uveitis (inflammation)
- Diabetes
- Trauma
- Congenital
What’s the treatment for cataracts?
The only treatment of cataract is cataract surgery. There is NO medical treatment of cataract.
The cataract surgery involves removal of cataract by ultrasonic energy (phacoemulsification) and implantation of a permanent intraocular lens (IOL).
There have been many advances in the development of special intra-ocular lenses that correct for astigmatism and presbyopia in addition to myopia and hyperopia. These advances have allowed patients to strive for spectacle independence. There are a variety of lens options available; it is important to have a frank discussion with your surgeon to assess your visual needs and expectations.
Best Eye Doctor For Cataract Surgery In Pathankot, Punjab
Saini Eye Hospital is the best hospital to get cataract surgery in the Pathankot district with advanced technology and minimum risks involved.
An end Swiss-made Phacoemulsification machine (Oertli) and a Japanese operating microscope (Takagi) are used to ensure 100 % precision.
Our surgeons are trained at the best eye hospitals in Delhi and provide the latest and world-class treatment options. MICS ( Micro Incision Cataract Surgery) is done in our hospital for all grades of cataracts. The surgery is completely painless and sutureless.
Lens implants
All types of lens implants are available to reduce the need for spectacles.
- Traditional Monofocal IOL
- EDOF (Extended Depth Of Focus) IOL
- Multifocal IOL
- Trifocal IOL
- Toric IOL